
Introduction
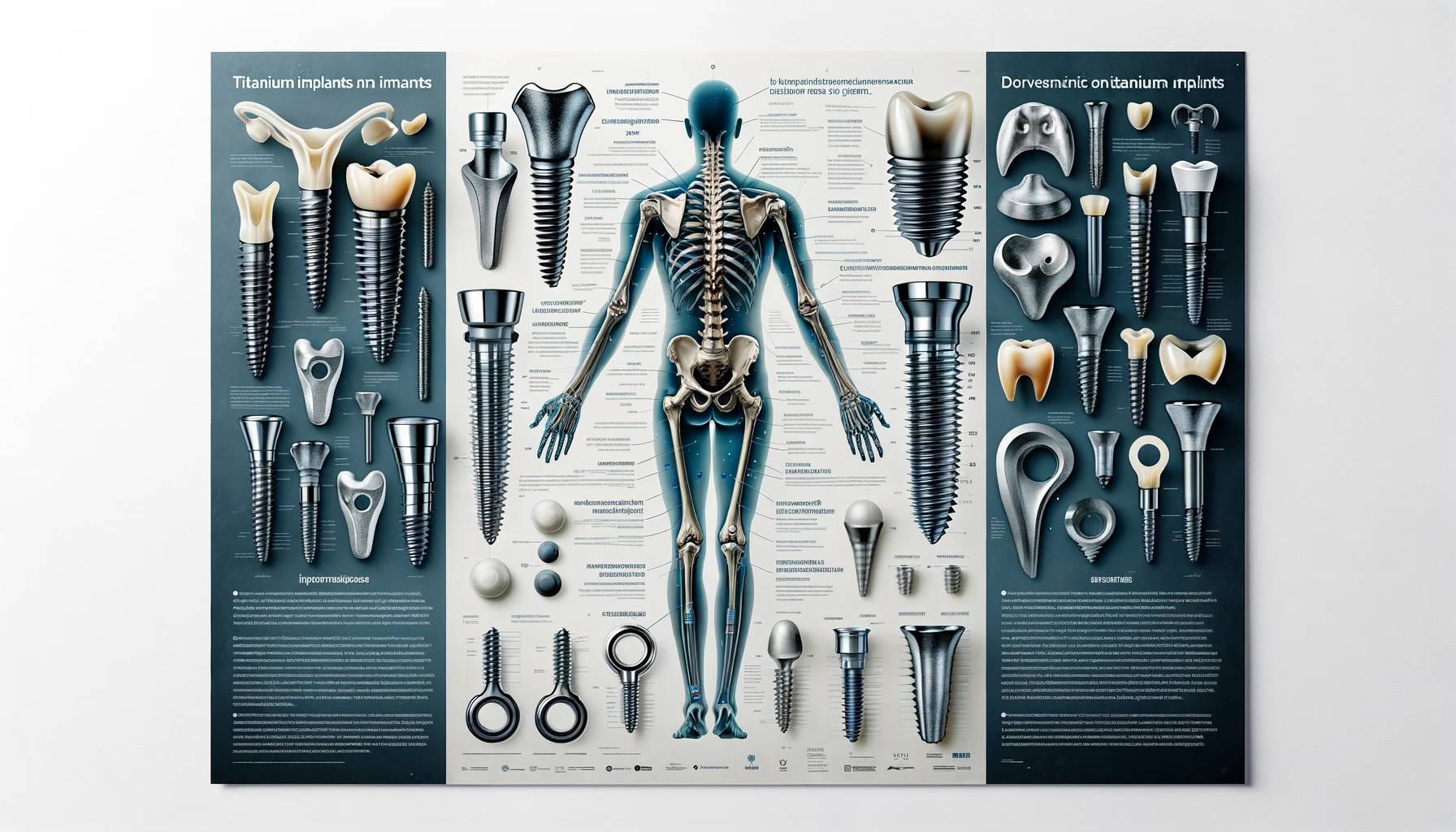
Titanium dental implants are a revolutionary solution in modern dentistry for replacing missing teeth. Crafted from high-grade titanium, a material known for its exceptional strength, biocompatibility, and ability to fuse with bone, these implants serve as a robust and long-lasting foundation for artificial teeth. The process involves surgically placing the implant into the jawbone, where it integrates with the bone tissue in a process known as osseointegration. This integration ensures a stable and durable base, upon which crowns, bridges, or dentures can be mounted, closely mimicking the look, feel, and function of natural teeth. Titanium implants have become highly favored due to their success rate, compatibility with body tissues, and the ability to prevent bone loss, making them a preferred choice for both dentists and patients seeking to restore their smiles.
Question 1
Why are implants made out of Titanium?
Implants are made out of titanium for several key reasons:
- Biocompatibility: Titanium is exceptionally biocompatible, meaning it is not harmful or toxic to living tissue. This is crucial for dental implants, as the material must exist in harmony with the body's natural tissues, particularly the bone and gums.
- Osseointegration Capability: Titanium has the unique ability to osseointegrate, or bond directly with bone. When a titanium implant is placed in the jawbone, over time, the bone cells grow around and attach to the implant surface, creating a strong, stable foundation for the artificial tooth. This osseointegration is vital for the long-term success and stability of the implant.
- Durability and Strength: Titanium is known for its high strength-to-density ratio. It's strong enough to withstand the biting and chewing forces in the mouth, yet it is also relatively lightweight. This makes it an ideal material for dental implants, which need to be both durable and not overly heavy or cumbersome.
- Corrosion Resistance: Titanium is highly resistant to corrosion by bodily fluids, which is essential for any material used inside the body. This resistance helps ensure the longevity of the implant and reduces the risk of degradation over time.
- Track Record of Success: Titanium has been used for dental implants for decades, and its success rate is well-documented. This long history of use has allowed dentists and researchers to refine implant techniques and confirms the material's effectiveness and safety.
These properties make titanium the material of choice for dental implants, providing a combination of strength, compatibility, and durability that is essential for the success of this type of dental restoration.
Question 2
What is osteoconduction?
Osteoconduction is a biological process that plays a crucial role in bone healing and regeneration, particularly in the context of bone grafts and implants like dental implants. The term refers to the ability of a material to serve as a scaffold or template along which new bone cells can grow. Here's a closer look at the concept:
- Scaffold for New Bone Growth: Osteoconductive materials provide a physical, 3D structure that facilitates the migration, growth, and attachment of osteoblasts (bone-forming cells) and other cells necessary for bone growth.
- Bone Healing and Regeneration: In the context of bone grafts or implants, osteoconduction allows new bone to grow on the surface of the graft or implant, which helps in integrating the graft material into the existing bone or in the case of implants, creating a strong bond between the implant and the bone.
- Importance in Dental Implants: For dental implants, especially those made of titanium, the osteoconductive property is vital. It aids in the process of osseointegration, where the jawbone grows around and bonds to the implant, creating a stable foundation for the artificial tooth.
- Use in Bone Graft Materials: Osteoconductive materials are also used in various bone graft materials, where they assist in repairing bone defects or augmenting bone in areas where bone mass is insufficient. These materials can be natural (like certain types of bone grafts) or synthetic (like hydroxyapatite or certain bioactive glasses).
- Not to be Confused with Osteoinduction: Osteoconduction is different from osteoinduction, another important process in bone healing. Osteoinduction involves stimulating immature cells to develop into pre-osteoblasts, which are precursor cells to bone-forming cells. Some materials and biological factors can promote both osteoconduction and osteoinduction.
In summary, osteoconduction is about providing a framework for new bone to build upon, essential in various orthopedic and dental procedures where bone healing and integration are needed.
Question 3
How is implant stability measured?
Implant stability is a critical factor in the success of dental implants and is measured using several methods:
- Periotest: The Periotest is an electronic device that measures the mobility of an implant. It works by gently tapping the implant and measuring the damping characteristics of the implant in the bone. Lower Periotest values indicate greater implant stability.
- Resonance Frequency Analysis (RFA): This is a widely used and non-invasive method for assessing implant stability. The RFA device, such as Osstell, attaches a small transducer to the implant, which is then excited to vibrate at its natural frequency. The resonance frequency is measured and converted into an Implant Stability Quotient (ISQ) value. Higher ISQ values (ranging from 1 to 100) typically indicate better stability.
- Torque Testing: Torque testing involves applying a rotational force to the implant. Initial stability is often assessed during implant placement by measuring the torque required to insert the implant. A higher insertion torque usually suggests better primary stability.
- Clinical Assessment: This involves manual testing of the implant stability by the clinician. It's more subjective and relies on the clinician's experience and judgment.
- Radiographic Evaluation: X-rays or other imaging techniques can be used to assess the bone-implant interface. Good osseointegration and absence of a radiolucent gap around the implant suggest stability.
- Cutting Torque Resistance Analysis (CRA): This method measures the torque resistance during implant placement and provides an indication of the bone density, which correlates with initial implant stability.
Each of these methods has its strengths and limitations. Often, clinicians use a combination of these techniques to get a comprehensive understanding of the implant's stability, which is crucial for determining the appropriate loading time and the long-term success of the implant.
Conclusion
In conclusion, titanium dental implants represent a significant advancement in dental restoration, offering a strong, durable, and biocompatible solution for replacing missing teeth. The choice of titanium is grounded in its unique properties, such as its ability to osseointegrate with the jawbone, providing unparalleled stability and longevity. Understanding the mechanisms like osteoconduction, which facilitate the integration and healing process, is essential in appreciating how these implants work and why they are so effective. Furthermore, the measurement of implant stability, through various techniques like Resonance Frequency Analysis and clinical assessments, plays a critical role in ensuring the success of the implant. These factors together underscore the sophistication and reliability of titanium dental implants as a restorative dental option, highlighting the synergy of material science and biology in modern dentistry.
Titanium is exceptionally biocompatible, meaning it is not harmful or toxic to living tissue.

.svg)
.svg)
.svg)