
Introduction
Tooth extractions are common at any age, but for older adults, they come with a unique set of challenges. One of the most dreaded complications following an extraction is something called dry socket—a painful condition that occurs when the protective blood clot in the socket either fails to form or becomes dislodged too early. While dry socket can happen at any age, studies and clinical observations show that older patients are at a significantly higher risk, especially when bone density is already compromised or when healing capacity has slowed due to age. But the concerns don’t stop at dry socket. As we age, our bone regeneration slows, and bone loss accelerates. That’s why many dentists recommend bone grafting after extraction, especially in seniors. A bone graft acts as a scaffold to preserve the ridge of the jawbone, maintain facial structure, and prepare for future treatments like dental implants or dentures. Without it, the area where the tooth was removed can collapse, making it much more difficult to restore later. What’s tricky is that most patients don’t realize how aging affects their healing process until complications happen. Many assume that because they healed well from extractions in their youth, the same rules will apply in their 60s, 70s, or 80s. Unfortunately, that’s not always the case. Factors like reduced blood flow, thinner gum tissue, and medications for common age-related conditions can all delay or disrupt proper healing—making older adults more vulnerable to post-extraction complications, including dry socket, infection, and severe bone loss. Another challenge is that symptoms of dry socket may be dismissed by older patients as “normal pain,” delaying treatment and worsening the outcome. Dry socket is not just discomfort—it’s intense, radiating pain that often starts a few days after the tooth is removed and may worsen instead of improving. In elderly patients, dry socket can significantly interfere with eating, speaking, and quality of life, especially if they’re already managing other health conditions. That’s where bone grafting comes in. It’s not just for aesthetics or future implants—it also provides immediate structural support to the area, helping to stabilize the socket and reduce the risk of dry socket by protecting the healing clot and preserving bone volume. It’s especially valuable in patients over 50, who may not heal as robustly as they once did. In this blog, we’ll explore: Why dry socket is more common and more severe in older adults The role bone grafting plays in preserving oral health as we age What older patients can do to promote safe healing and reduce complications after an extraction Whether you’re preparing for a tooth extraction yourself, helping a parent or loved one understand their options, or simply want to be proactive about your oral health as you age, this guide will provide the facts and insights you need to make informed decisions.
Question 1
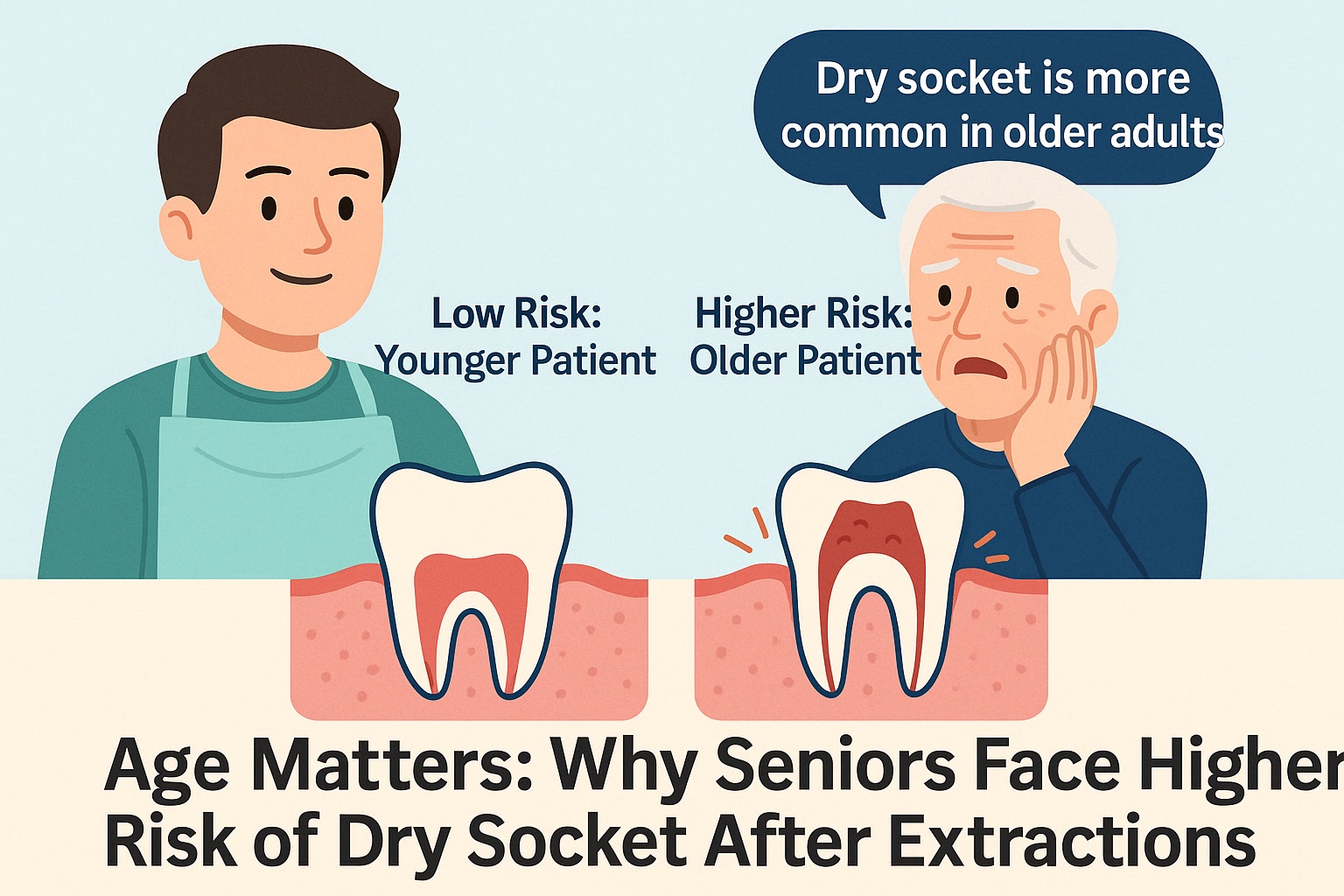
Why Are Older Adults More Likely to Experience Dry Socket After a Tooth Extraction?
Dry socket, or alveolar osteitis, is one of the most painful complications following a tooth extraction. It occurs when the blood clot that should naturally form inside the socket either dissolves too early or becomes dislodged, leaving the bone and nerves exposed. This results in significant, radiating pain—often to the ear or temple—and a delayed healing process. While anyone can develop dry socket, older adults face a significantly higher risk, and understanding why is crucial to preventing it.
One of the main reasons age increases dry socket risk is reduced blood supply. As we age, the vascular system that supports gum tissue and bone becomes less efficient. Blood doesn’t flow as quickly or as abundantly to surgical sites, meaning the clot that forms after an extraction may not stabilize as well. This makes it more vulnerable to breaking down or being lost, which sets the stage for dry socket.
Another factor is bone density and quality. Older patients often experience age-related bone loss, especially postmenopausal women and those with osteoporosis. This can make the jawbone more fragile and less likely to produce the rich matrix needed to support clot formation and healing. Bone that has already resorbed or is compromised from periodontal disease is less likely to heal predictably after an extraction.
Medications are another major contributor. Many seniors are on blood thinners, bisphosphonates (for osteoporosis), steroids, or medications for diabetes or autoimmune conditions. These drugs can slow clotting, reduce bone turnover, or impair immune response, which raises the risk of infection and dry socket formation. Some medications, like bisphosphonates, also create long-term changes in how bone remodels—making post-extraction recovery more complex.
Salivary flow is another issue often overlooked. Dry mouth is more common in seniors, due to medications, systemic conditions, or simply age-related changes in the salivary glands. Saliva plays an important role in protecting oral tissues, lubricating the socket, and aiding in clot stabilization. When the mouth is dry, there's more friction and less natural healing support, further increasing dry socket risk.
In addition, older patients may have difficulty following post-operative instructions perfectly. Whether due to cognitive issues, physical limitations, or misunderstanding, failure to avoid certain activities like rinsing, spitting, or drinking through a straw can unintentionally dislodge the blood clot and trigger dry socket.
And finally, aging gums are thinner and more fragile. This makes the surgical site more delicate and prone to trauma, whether from brushing, eating, or just talking. Without the robust tissue protection that younger patients enjoy, the healing socket in a senior patient is more exposed and susceptible to complications.
The good news is that understanding these risks means they can be managed. With the right precautions and support, older patients can still recover comfortably after an extraction—but it requires a more customized, cautious approach. In the next section, we’ll look at how bone grafting can support healing and reduce complications for aging patients.
Question 2
Is Bone Grafting More Important for Older Adults After Tooth Extraction?
Absolutely—and here’s why. Bone grafting after a tooth extraction helps preserve the structure of the jawbone and socket by providing a scaffold that supports bone regeneration. While this is beneficial at any age, it becomes even more important in older adults due to faster bone loss, slower healing, and reduced natural regenerative capacity.
When a tooth is removed, the surrounding bone begins to shrink or "resorb." This happens because the body no longer needs to maintain bone that doesn’t support a tooth. In younger patients, the body may naturally regenerate some of that bone. But in older adults—especially those over 50—bone regeneration slows dramatically. That means bone volume is lost more quickly and more permanently unless something is done to intervene.
Bone grafting provides that intervention. It introduces a mineral-based or biologically active material into the socket immediately after extraction, which serves as a scaffold for new bone cells to attach, grow, and rebuild. For older adults, this is crucial because the native bone may not grow back on its own—and once it’s gone, it becomes much harder (or impossible) to place a future implant or denture securely.
There’s another benefit to grafting in seniors: it helps protect the healing socket and reduce dry socket risk. How? Bone grafting stabilizes the area and provides volume to support clot retention. This helps keep the blood clot in place longer, shielding the underlying bone and nerves while the area heals. It also creates a physical buffer between the exposed socket and outside elements like food, air, and bacteria, which reduces irritation and improves healing.
Older patients are also more likely to need prosthetic replacements for missing teeth, such as dentures or implants. Without bone grafting, the ridge where the tooth used to be can collapse, resulting in a sunken-in appearance, poor denture fit, or the inability to get an implant at all. In this sense, grafting isn’t just about recovery—it’s about preserving long-term options and oral health functionality.
Furthermore, as we age, our bodies respond more slowly to trauma, and infection risk increases. A grafted site is often better supported during the early stages of healing, helping reduce the chance of post-extraction infections and inflammation that can further degrade bone or tissue.
Some older patients are hesitant to accept a bone graft due to cost, concerns about healing, or the perception that it's unnecessary at their age. But from a clinical standpoint, bone grafting is often more critical for older adults than for younger ones, precisely because their healing potential is reduced. It’s a form of preventive medicine—protecting the socket today to prevent problems tomorrow.
At KYT Dental Services, we often recommend socket preservation grafts for our aging patients, especially those with pre-existing bone loss, systemic health issues, or plans for future implants. It’s a simple, in-office procedure that dramatically improves long-term outcomes and reduces complications.
Question 3
How Can Older Adults Prevent Dry Socket and Support Healing After Extraction?
The good news is that while older adults are at higher risk for dry socket, there are many ways to reduce that risk and promote safe, comfortable healing. The key is combining surgical techniques with smart post-operative care and personalization based on health history.
First and foremost, older patients should consider a socket preservation bone graft. As discussed earlier, this provides support for the healing site and helps maintain bone structure while reducing dry socket risk. But beyond grafting, the dentist’s surgical technique plays a big role too. Gentle extraction methods, PRF (platelet-rich fibrin), and careful socket irrigation all contribute to a more stable healing environment.
Once the tooth is removed, post-op instructions become critical—especially in the first 24–72 hours. Older patients or their caregivers should be given very clear written and verbal guidance that includes:
- Do not smoke or vape (nicotine greatly increases dry socket risk)
- Avoid drinking through a straw
- Don’t rinse vigorously or spit for the first 48 hours
- Stick to soft foods and avoid hot liquids early on
- Keep the head elevated during rest
Older adults with medical conditions or medications that affect clotting (like blood thinners) may need pre-surgical medical clearance or adjusted protocols to promote clot stability. This can include using hemostatic agents, gauze packs, or clot-preserving materials.
Hydration also matters. Seniors with dry mouth are more vulnerable, so drinking water regularly (once safe to do so post-surgery) and using saliva substitutes if needed can support tissue health.
Patients with slower healing should also ask about platelet-rich fibrin (PRF), a regenerative technique that uses the patient’s own blood to create a healing membrane placed over the socket. This method is highly biocompatible and helps reduce inflammation, encourage faster healing, and minimize dry socket risk—especially in patients with compromised immune function or poor circulation.
Dental teams should follow up proactively. Older adults may hesitate to report pain, assuming it’s normal. A quick follow-up call or a 48-hour check-in can catch signs of dry socket early before it becomes a serious issue. Caregivers should be trained on what to look for—persistent pain, bad breath, or an empty-looking socket are common red flags.
Finally, nutritional support matters. Older patients healing from extractions should prioritize foods rich in vitamin C, protein, and zinc—all of which help with tissue repair. Gentle saltwater rinses (after 72 hours) may help keep the area clean, but only if the clot is stable.
In summary, dry socket in older adults is preventable—but it requires more intentional planning. Bone grafting, surgical technique, medication review, post-op support, and follow-up all play a role in ensuring seniors recover safely. With the right precautions, aging patients can experience a smooth healing process without pain, infection, or long-term complications.
Conclusion
Tooth extractions are a routine dental procedure, but for older adults, they require a deeper level of consideration and planning. The risk of dry socket—a painful complication caused by the loss of the protective blood clot—is significantly higher in seniors due to a combination of age-related biological changes. Slower healing, reduced blood flow, medication interference, and bone density loss all contribute to making post-extraction recovery more fragile in this population. But this doesn’t mean tooth extractions should be avoided as we age. On the contrary, addressing dental problems in a timely and proactive way is critical to maintaining long-term oral and systemic health. The key is understanding the risk factors and adjusting the treatment approach accordingly. That’s where bone grafting, personalized surgical techniques, and post-operative care plans make all the difference. For older patients, bone grafting after an extraction isn’t just optional—it’s often essential. As the body’s natural ability to regenerate bone slows down, socket preservation becomes a necessary step to maintain the ridge structure, prevent facial collapse, and protect future restorative options like implants or dentures. Without it, the socket can resorb rapidly, leaving less bone to work with and increasing the risk of complications like dry socket or infection. It’s also important to acknowledge that many older patients are taking medications—such as blood thinners, bisphosphonates, or immunosuppressants—that affect healing and clot stability. That’s why dental offices must be proactive about medical history reviews and obtain medical clearance when appropriate. For patients with complex health needs, even a simple extraction becomes a multi-layered event requiring coordination and caution. The good news is that there are many tools available today to make recovery safer and more predictable. Using techniques like platelet-rich fibrin (PRF), gentle surgical methods, and supportive materials like collagen plugs or resorbable membranes can help protect the clot and improve tissue repair. Just as importantly, a well-structured post-operative care plan—tailored to the specific needs and risks of an older patient—can make a dramatic difference in healing outcomes. Older adults also benefit from closer follow-up. Sometimes, discomfort that might signal dry socket is brushed off as normal aging or ignored until it becomes severe. A dental team that prioritizes patient education, gentle communication, and proactive check-ins can catch issues early and prevent unnecessary pain or complications. Ultimately, age shouldn’t be seen as a barrier to dental care—it should simply influence how that care is delivered. With the right approach, older patients can have extractions, bone grafts, and restorations that are just as successful and comfortable as those performed in younger populations.
The risk of dry socket—a painful complication caused by the loss of the protective blood clot—is significantly higher in seniors due to a combination of age-related biological changes.

.svg)
.svg)
.svg)